Period tracking apps: What you need to know

Period tracking apps are easy to access via your app store on any smartphone. You might have heard of ones like Cycles, Glow, Eve, or Flo. Most period tracking apps get you to enter some information regularly, like the days that you are bleeding, and any other period-related symptoms you might have. After a few cycles, the app should show you information such as how long your cycles last, on average.
There are many ways period tracking apps can help you monitor your reproductive health:
- Track your cycle and predict your next period
- Understand when you might ovulate and are most fertile
- Remind you when to take oral contraceptive pills
- Measure your heart rate and basal body temperature
- Track your cervical mucous and PMS symptoms
- Track days you have been sexually active
- Some apps can also track pregnancies
Period tracking apps are growing in popularity, as people find it convenient to track their cycle with more precision, and know more about their bodies. However, some people are also using these apps to prevent pregnancy, possibly to avoid having to use contraceptive devices or medications.
Period trackers aren’t always great at preventing pregnancies.
Using a period tracking app for contraception is only 75% effective. This means that for every 100 women that use a tracking app to avoid pregnancy, 25 will become pregnant. For comparison, a contraceptive implant is over 99% effective.
Some apps will alert you in some way (eg. Highlight your calendar or change colour) to tell you to when you are fertile or not. These timeframes may not be inaccurate and you might become pregnant. If you have an irregular period, are not an organised person, or become unwell, the app may not accurately track your cycle.
Even apps like Natural Cycles that make you record your ‘basal body temperature’ everyday are not always accurate. Your basal body temperature is your body temperature during rest; for many people, there is a slight increase in basal body temperature when you ovulate. However, using your body temperature to estimate your ovulation dates can be risky; accurate estimates require you to measure your temperature at exactly the same time every day, immediately as you wake up. Furthermore, your body temperature can also be affected by things like sickness, stress, smoking, alcohol, medications or the weather.
Some studies have found that ‘basal body temperature’ tracking methods are only 22% effective at tracking ovulation, which could have led to unplanned pregnancies. One hospital in Sweden found that 37 of 668 patients seeking abortion had been relying on Natural Cycles, and the UK advertising watchdog cautioned the company for having misled consumers, and “exaggerated the efficacy of the method as a form of contraception.”
Period tracking apps and your health data
Generally, health apps are a multimillion industry and period tracking apps are no exception. Some apps are free, while others might have a fee where you enter payment and a monthly fee thereafter. Because apps are big business for marketers and medical companies, consider the benefit of the app for your health and wellbeing before committing to a purchase. Remember to check what the app might do with your health information – will it be secure? (For example, in 2021, the period tracking app Flo ‘settled a complaint with the FTC which alleged that the company was selling users’ health data to Facebook and Google, as well as marketing and analytics firms’.) You can find out more about popular fertility apps and your privacy here.
The bottom line
Period tracking apps can be useful for lots of things, like predicting your next bleed or tracking your period-related symptoms. However, they are not the most effective form of contraception, and can’t protect you against STIs.
If you want discuss all your contraception options, contact our team on 1800 696 874 (weekdays, 9am – 5pm) or search for a contraception provider online.












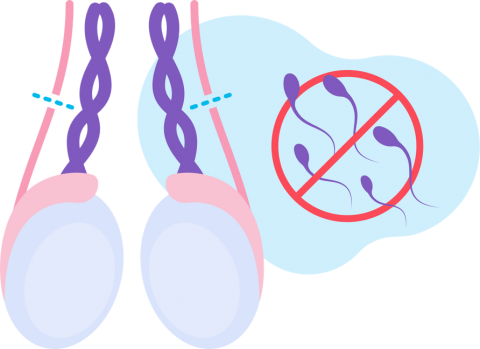 The vas deferens are cut and tied, or sealed, to prevent sperm from travelling from the testicles to the penis.
The vas deferens are cut and tied, or sealed, to prevent sperm from travelling from the testicles to the penis. 


